Emergency and General Healthcare
Emergency and General Healthcare
Can Dogs Have Asthma?
 Karissa
Karissa
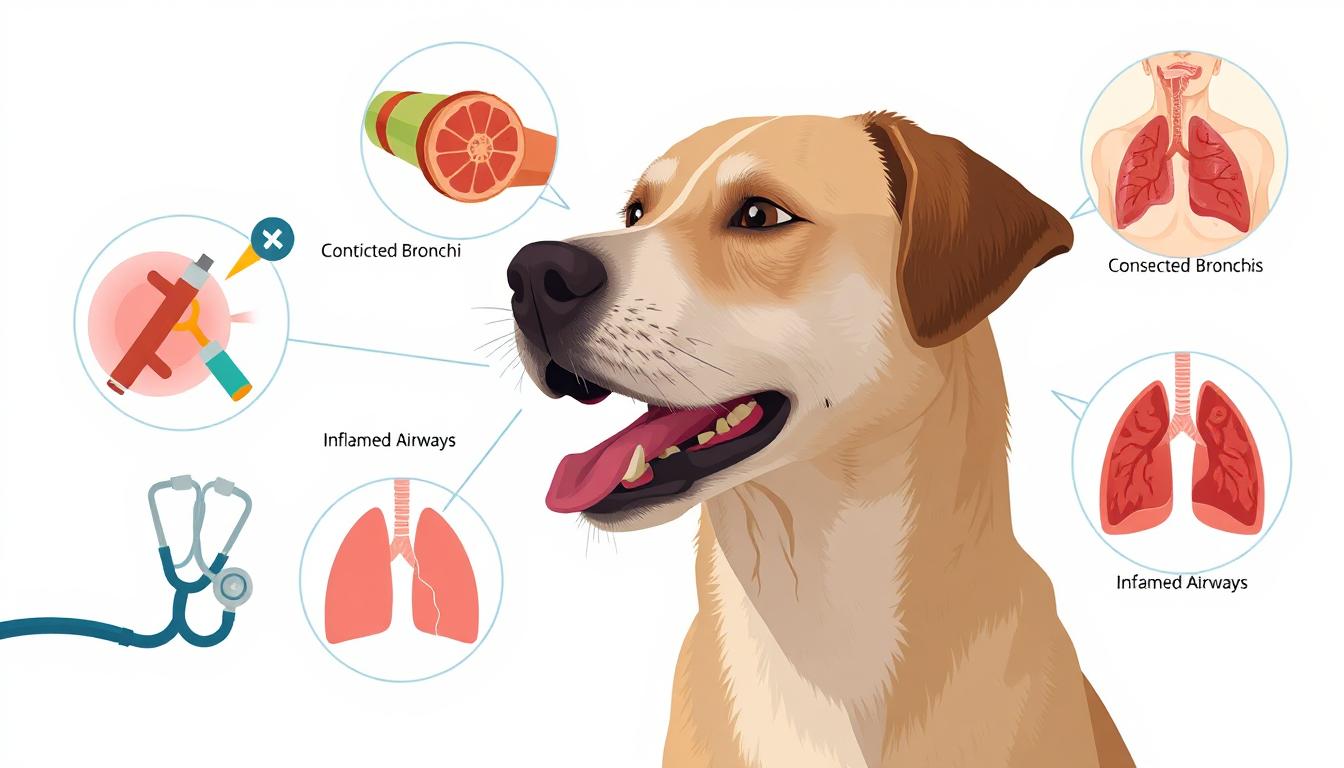
Canine Asthma: A Real but Rare Diagnosis Many puppy owners are surprised to know that canine allergies are a valid state, yet less common in dogs than in humans. Canine allergies, commonly referred to as allergic bronchitis or chronic bronchial inflammation, can lead to human asthma, which is characterized by cough, difficulty breathing, labored breathing, or lethargy. While it is more popular among small species and older dogs, any dog can develop this condition if environmental triggers such as dust, mold, smoking, or pollen are contacted. It is important to recognize those signs and consult a veterinarian as soon as your dog gets urgent care. Use the correct asthma ICD 10 code when seeking insurance claims or documenting your diagnosis. Understanding Asthma in the Genetic and Environmental Context The question "Is allergic genetic?" There is a common subject in both human and veterinary medicine. In puppies, as in humans, genetic tendency can additionally play a role. Some breeds, such as pugs and bulldogs, are more prone to their narrow airways. However, dog bronchial asthma is usually exacerbated or aggravated by environmental factors.Smokers or homes with excessive pollen levels can also inadvertently exacerbate a pet's condition. Understanding the interplay between heredity and surroundings is critical in growing a bronchial asthma-safe space for your canine. Is asthma genetic? Yes, genetics can play a role, especially if there’s a family history of asthma or allergies. Diagnostic Tools: How Veterinarians Confirm Asthma Just as with human instances recognized under the asthma ICD-10 coding system, diagnosing canine allergies requires thorough evaluation. Veterinarians may also perform chest x-rays, listen for wheezing, and verify respiration patterns. Can asthma go away? In some children, asthma may improve with age, but in most cases, it requires long-term management.A bronchial asthma control test adapted for puppies can contain workout response and symptom frequency logging. While no unmarried blood test confirms allergies, ruling out infections or parasites is a part of the diagnostic technique. Pet proprietors must display coughing episodes and note any correlation with environmental adjustments or strain. Treatment Tools: Inhalers and Nebulizers for Dogs For extreme instances, puppies might also require breathing help via devices similar to human allergy machine setups. Nebulizers deliver bronchodilators and corticosteroids simultaneously to the lungs, reducing irritation and opening airways. Some dogs can also use specially designed dog masks that fit over their snout. While over-the-counter asthma inhaler alternatives exist for people, these are not safe for puppies unless prescribed by a veterinarian. Administering a human OTC asthma inhaler to a canine can be dangerous without veterinary oversight. An asthma machine, or nebulizer, turns liquid medication into mist for easier breathing in children and adults. Family Allergy and Asthma Risks Extend to Pets It’s not uncommon for households with persistent respiratory situations to marvel about shared allergens. Clinics consisting of Family Allergy and Asthma have documented how shared environments can have an effect on both humans and animals. Family Allergy and Asthma clinics specialize in diagnosing and treating allergic conditions and asthma in all age groups.If your toddler or partner is suffering from asthma, your dog will also be struggling silently. Monitoring air quality, disposing of scented merchandise, and using HEPA filtration can enhance outcomes for every respiratory member of the family, four-legged or not. Can Asthma Go Away in Dogs? Managing Chronic Symptoms A generally asked question is: “Can bronchial asthma depart?” In dogs, allergies are considered a persistent circumstance, just like in humans. While signs and symptoms may be managed or decreased through the avoidance of triggers and medication, a lasting remedy is unlikely. That said, many dogs live full, lively lives with proper allergy management. Treatment may also include corticosteroids, bronchodilators, and lifestyle modifications. Working closely together with your veterinarian ensures that your puppy’s symptoms remain managed. An over the counter asthma inhaler may offer short-term relief, but most effective treatments require a prescription. Asthma Control Test for Dogs: A Holistic Monitoring Approach Although no longer equivalent to the human asthma control test, pet owners can report symptom frequency, severity, and exposure to triggers to assess the effectiveness of manual treatment. Keep a log of cough episodes, breathing modifications, or use of medicinal drugs. An OTC asthma inhaler can provide temporary relief but isn’t a substitute for long-term asthma control therapy.Share this log along with your allergies, health practitioner, or veterinarian to tailor a remedy. This proactive approach ensures ongoing well-being and stops emergency conditions, particularly during hypersensitive reaction seasons. Should You Use an OTC Asthma Inhaler on Dogs? The growing reputation of OTC bronchial asthma inhaler options has led a few puppy owners to test self-medicating their puppies. This is surprisingly discouraged. Dog asthma is a condition where dogs experience wheezing, coughing, and labored breathing due to airway inflammation.Human dosages and shipping mechanisms are not calibrated for animals. Using an over-the-counter asthma inhaler on a canine without expert supervision could cause overdose, an extended heart rate, or ineffective relief. Always consult your pet’s asthma physician before introducing any remedy. Asthma Machines and Canine Respiratory Therapy For more intense or persistent cases, a home asthma machine along with a nebulizer may be encouraged. These devices help deliver a pleasant medicinal mist directly into the airways through a fitted mask. Dogs regularly tolerate these remedies better than oral medications, and they provide quicker relief in some stage of acute episodes. Regular use can save you and enhance oxygenation. Reliable nebulizers and breathing assist devices can be located at SanfordPharmacy.com, where both human and pet health answers are available. An asthma doctor, often a pulmonologist or allergist, helps create personalized treatment plans to manage your symptoms. Conclusion: Breathe Easy, Together Dog asthma is a manageable condition if diagnosed early and treated correctly. While allergies are genetic, environmental control, proper medication, and vigilant observation are the pillars of dog respiratory fitness. The asthma control test is a questionnaire that helps evaluate how well your asthma is being managed.Avoid using OTC bronchial asthma inhaler products without guidance, and consult your vet on analog treatment plans. Whether you are managing allergies for yourself, your child, or your reliable canine partner, go to sanfordpharmacy.com for prescription drugs, respiratory equipment, and respiratory health products you may need.

Emergency and General Healthcare
what is the correct order of steps of the pediatric out of hospital chain of survival
 Gilbert
Gilbert
Timely and precise motion can imply the difference between lifestyles and death in pediatric emergencies. The pediatric out-of-clinic chain of survival is a structured sequence designed to optimize results for youngsters experiencing lifestyles-threatening events outside clinical settings. Each hyperlink in this chain requires preparedness, fast decision-making, and a combination of pediatric information. Step 1: Prevention and Early Recognition The foundation of pediatric survival lies in vigilance. Parents, caregivers, and medical professionals play critical roles in spotting early warning symptoms and minimizing environmental risks. Preventive care from professionals such as a pediatric gastroenterologist or pediatric endocrinologist can lessen the hazard of crises related to chronic or metabolic disorders. Routine screenings with a pediatric eye doctor can also reveal neurological or systemic conditions before they become emergencies. Through collaborative preventive care, many pediatric emergencies can be avoided completely. Step 2: Immediate Activation of Emergency Response When an emergency occurs, the second hyperlink is fast activation of the emergency response machine. The pediatric assessment triangle—evaluating look, respiration, and flow—serves as a frontline device for identifying life-threatening conditions.Once a serious problem is suspected, prompt contact with emergency services is vital. Community awareness of when and how to call for assistance must be emphasized, in particular in houses and establishments caring for medically vulnerable children. Step 3: High-Quality CPR Cardiopulmonary resuscitation should be initiated immediately if the child is unresponsive and no longer breathing. The anatomical and physiological variations in youngsters necessitate a modified approach to CPR.Parents and caregivers are encouraged to undergo pediatric CPR education, which is regularly available through centers like PM Pediatric Urgent Care. Equipping bystanders with these capabilities bridges the distance before professional responders arrive. Step 4: Rapid Defibrillation (If Indicated) Although less common in youngsters than adults, surprising cardiac arrest due to arrhythmias nonetheless occurs, mainly in undiagnosed congenital heart conditions. In these instances, early defibrillation is essential.AEDs equipped with pediatric pads should be available in faculties, community facilities, and even the homes of at-risk kids. Bystanders ought to be educated on proper AED use to ensure this life-saving step isn't always behind schedule. Step 5: Effective Advanced Life Support As emergency clinical experts arrive, the transition to advanced existence help (ALS) starts. ALS includes airway management, IV get right of entry to, medication management, and cardiac tracking tailor-made to pediatric physiology.This step underscores the value of fast and seamless handoff from bystanders to educated responders—each performing inside their scope of functionality to stabilize the kid for transport. Step 6: Integrated Post-Cardiac Arrest Care Recovery doesn’t give up with resuscitation. Post-cardiac arrest care includes stabilizing vital symptoms, stopping further organ damage, and making plans the transition to definitive care. Transport teams work to preserve neurological function and ensure minimal postpone in achieving pediatric-capable centers.At this stage, collaborative input from subspecialists becomes important. Whether it is a pediatric orthopedic medical professional coping with trauma, a pediatric dermatologist treating skin headaches from burns or hypersensitive reactions, or a pediatric ENT addressing airway injuries, specialized care is vital. The Role of Pediatric Specialists in Recovery Children convalescing from essential occasions frequently require ongoing care from a network of professionals. A pediatric medical professional can also intervene in stressful or congenital instances, whilst lengthy-term healing might also involve pediatric physical therapy to restore characteristic and mobility.The involvement of a pediatric endocrinologist is crucial while hormonal or metabolic triggers contribute to the emergency. Similarly, gastrointestinal distress connected to systemic situations may necessitate follow-up with a pediatric gastroenterologist.Together, these specialists form a complete care surroundings that addresses each the instant aftermath and lengthy-term health of the pediatric patient. Access to Trusted Medications and Support Reliable access to remedy is a cornerstone of pediatric put up-emergency care. Families navigating complicated remedy regimens should flip to depended on resources for their pharmaceutical desires.SanfordPharmacy.Com offers a full spectrum of pediatric medicines—from antibiotics and ache relievers to strong point prescriptions required with the aid of pediatric gastroenterologists, pediatric endocrinologists, and extra. With stable delivery and easy online ordering, it ensures continuity of care for every child’s restoration adventure. Conclusion Understanding the correct order of steps in the pediatric out-of-medical institution chain of survival empowers caregivers and groups to act decisively in vital moments. From prevention to rehabilitation, every phase requires tailored motion and expert care. For safe, reliable access to all essential drug treatments and pediatric help merchandise, families are endorsed to rely on SanfordPharmacy.Com a partner for your baby’s fitness, each step of the way.

Emergency and General Healthcare
What is the Correct Order of Steps of the Pediatric Out of Hospital Chain of Survival?
 Cassidy
Cassidy
Disclaimer:Content on Sanford Pharmacy is meant for general information and should not be seen as medical advice. Please consult a licensed healthcare provider before using any medicine. Self-treatment without guidance is not recommended. When a pediatric emergency happens outside the hospital, fast reaction and proper intervention can imply the difference between life and demise. Searching for a pediatric dermatologist near me? Sanford Pharmacy provides information on trusted pediatric dermatologists in your area.The Pediatric Out-of-Hospital Chain of Survival is a hard and fast of critical steps designed to grow survival prices for kids experiencing cardiac arrest or respiration failure. A pediatric dermatologist specializes in diagnosing and treating skin conditions in infants, children, and adolescents. Unlike adults, pediatric cardiac arrests are frequently because of respiratory troubles rather than coronary heart disease, making early intervention and rescue respiratory vital. The pediatric assessment triangle is a rapid evaluation tool used by healthcare providers to assess a child's condition based on appearance, work of breathing, and circulation.Whether you’re a pediatric CNA, nurse, or caregiver, expertise in these steps is essential in emergencies. A pediatric cardiologist diagnoses and treats heart conditions in children, from congenital defects to arrhythmias.In this manual, we’ll destroy down:✅ The correct order of steps in the Pediatric Chain of Survival✅ Key variations between pediatric and personal resuscitation✅ Recognizing pediatric cardiac and breathing emergencies✅ The position of CPR, chest compressions, and defibrillationLooking for pediatric dentistry near me? Sanford Pharmacy connects you with reputable pediatric dental clinics in your vicinity. What Is the Correct Order of Steps within the Pediatric Out-of-Hospital Chain of Survival? The Pediatric Chain of Survival consists of five essential steps to ensure the highest possibilities of survival in out-of-sanatorium pediatric emergencies. Little Spurs Pediatric Urgent Care offers immediate medical attention for children with non-life-threatening conditions.1️⃣ Prevention and Early Recognition – Identifying respiratory distress and performing quickly2️⃣ Early Activation of Emergency Response – Calling 911 for instant assist3️⃣ High-Quality CPR – Providing powerful chest compressions and rescue respiratory4️⃣ Rapid Defibrillation (if wished) – Using an AED (automated external defibrillator) for shockable rhythms5️⃣ Advanced Life Support and Post-Resuscitation Care – Provided with the aid of paramedics and medical institution teamsEach of those steps works together to maximize survival and reduce headaches. A pediatric ENT (Ear, Nose, and Throat) specialist addresses issues like ear infections, tonsillitis, and sinus problems in children. Understanding the Pediatric Chain of Survival Unlike adults, pediatric cardiac arrest is most often resulting from respiration failure rather than underlying heart conditions. A pediatric eye doctor specializes in diagnosing and treating vision problems and eye diseases in children. This means:✔️ Early airway management and rescue respiration are vital✔️ Prompt activation of emergency offerings can prevent deterioration✔️ CPR for children includes more emphasis on rescue breathsThe aim of the Pediatric Chain of Survival is to intervene early before cardiac arrest takes place, making sure there are higher long-term results. Recognizing pediatric headache red flags, such as sudden severe pain or headaches accompanied by vomiting, is crucial for timely medical intervention.Key Differences Between Pediatric and Adult Chain of SurvivalWhile the Adult Chain of Survival focuses commonly on surprising cardiac arrest, the Pediatric Chain prioritizes breathing help and early intervention. The pediatric nurse salary varies based on experience, location, and healthcare settings, with competitive compensation reflecting their specialized skills. Aspect Pediatric Chain of Survival Adult Chain of Survival The Most Common Cause of Arrest is Respiratory failure, Cardiac diseaseCPR Emphasis 30:2 ratio with precedence on rescue respiration 30:2 ratio with recognition on chest compressionsDefibrillation is Used if a shockable rhythm is a gift, but it is much less common. It is often required in sudden cardiac arrest. PM Pediatric Urgent Care provides specialized after-hours medical services tailored for children and adolescents.Emergency Activation If by myself, provide 2 minutes of CPR first, then call 911. Pediatric physical therapy focuses on improving motor skills, balance, and strength in children with developmental or physical challenges.Call 911 without delay, then begin CPR.Recognizing Pediatric Cardiac Arrest and Respiratory Emergencies. A pediatric CNA (Certified Nursing Assistant) provides basic care and assists with daily activities for pediatric patients under the supervision of registered nurses.Early reputation is prime in pediatric emergencies. Warning symptoms consist of:🚨 Signs of Pediatric Respiratory Distress:📌 Rapid respiration or gasping📌 Nasal flaring📌 Retractions (seen pulling in of chest muscle tissue with respiratory)📌 Cyanosis (bluish skin, lips, or fingernails)🚨 Signs of Pediatric Cardiac Arrest:📌 Unresponsiveness📌 No everyday breathing📌 Weak or absent pulseHealthcare providers, which includes those running in PM Pediatric Urgent Care, pediatric bodily therapy, or pediatric occupational therapy, need to learn to understand those signs and symptoms early. A pediatric gastroenterologist treats digestive system disorders in children, including issues like chronic abdominal pain and inflammatory bowel disease. The Importance of Early Intervention in Pediatric Emergencies Pediatric occupational therapy assists children in developing the skills necessary for daily living and academic success. Early intervention can save you from complete cardiac arrest. This is mainly critical in instances involving:📌 Pediatric Headache Red Flags – Headaches observed through vomiting, confusion, or seizures may additionally suggest a neurological emergency.📌 Pediatric Gastroenterology Issues – Severe dehydration from diarrhea or vomiting can cause shock.📌 Pediatric Eye Conditions – Sudden vision loss or eye trauma calls for pressing evaluation by using a pediatric eye medical doctor.Recognizing early warning symptoms permits instant movement, enhancing survival chances. Parents looking for a pediatric dermatologist near me can rely on Sanford Pharmacy to find expert skin care professionals for their children. How Emergency Response Systems Work for Pediatric Cases 🚑 When calling 911, be prepared to offer:✔️ Child’s age and weight✔️ Signs of misery (respiratory or pulse troubles)✔️ Whether CPR is in development✔️ Medical records (if recognized)Pediatric emergencies require specialized care, so paramedics may additionally deliver advanced pediatric equipment for transport to the health center. Consulting a pediatric dermatologist ensures that your child receives specialized care for various skin issues. Understanding the Role of CPR in Pediatric Resuscitation CPR is crucial in pediatric emergencies, as it continues oxygen flowing to important organs. The American Heart Association (AHA) recommends:✔️ Chest compressions: 1.5-inch depth for babies, 2-inch depth for children✔️ Compression rate: 100-120 compressions according to minute✔️ Rescue breaths: 2 breaths after each of 30 compressions (or 15:2 if rescuers are present)If low unfastened testosterone is suspected in adolescent men because of endocrine problems, this could increase the chance of fatigue and negative movement, similarly complicating resuscitation efforts. Understanding the pediatric assessment triangle helps in promptly identifying and addressing pediatric emergencies. The Importance of Chest Compressions and Rescue Breathing Pediatric CPR differs from adult CPR due to the fact youngsters frequently go through hypoxia (low oxygen levels) before cardiac arrest.✔️ Chest compressions preserve the coronary heart-pumping✔️ Rescue breaths offer needed oxygen to the lungsIf completed early, CPR can double or triple survival charges. Parents seeking a pediatric cardiologist can consult Sanford Pharmacy for referrals to experienced heart specialists for children. Defibrillation and Its Role in Pediatric Cardiac Arrest While defibrillation (using an AED) is vital for adult sudden cardiac arrest, it's miles much less common in pediatric cases. However, an AED has to nonetheless be used if:✅ The toddler has no pulse and is unresponsive✅ A shockable rhythm (ventricular traumatic inflammation or pulseless ventricular tachycardia) is detectedAEDs with pediatric pads are advocated, but person pads may be used if pediatric settings are unavailable. For families searching for pediatric dentistry near me, Sanford Pharmacy offers guidance on finding child-friendly dental care providers. Defibrillation and Its Role in Pediatric Cardiac Arrest Defibrillation is a life-saving intervention used to deal with shockable cardiac rhythms like ventricular traumatic inflammation (VF) and pulseless ventricular tachycardia (VT). Parents trust Little Spurs Pediatric Urgent Care for prompt and specialized pediatric services without the long wait times.📌 When is defibrillation needed in pediatrics?🔹 Pediatric cardiac arrest is most often because of respiration failure, but in instances of VF/VT, an automated external defibrillator (AED) should be used.🔹 An AED with pediatric pads and settings is ideal, but if unavailable, grownup pads can be used, ensuring they no longer overlap.🔹 The encouraged energy dose for pediatric defibrillation is two J/kg for the first surprise, growing to 4 J/kg for subsequent shocks.📌 Defibrillation key factors:✔️ Early CPR + defibrillation can double or triple survival rates.✔️ Children under eight years old have to use pediatric-unique AED settings.✔️ If a shockable rhythm is detected, defibrillation has to be administered ASAP.Consulting a pediatric ENT ensures comprehensive care for your child's ear, nose, and throat health concerns. How Emergency Medical Services (EMS) Provide Pediatric Care 🚑 When EMS arrives, they ought to swiftly investigate and offer crucial interventions, consisting of:🔹 Using the Pediatric Assessment Triangle (PAT) – A quick visual device for assessing appearance, respiration, and stream.🔹 Providing oxygen and air flow – Ensuring the airway is obvious and oxygenated.🔹 Initiating exceptional CPR – With an emphasis on both compressions and ventilations.🔹 Defibrillation if needed – Using a pediatric-suitable AED.🔹 Administering medications – Epinephrine and different advanced existence assist (ALS) remedies.🔹 Rapid delivery to a pediatric emergency facility – Such as Little Spurs Pediatric Urgent Care or a pediatric sanatorium.The speed and performance of EMS groups play an essential position in enhancing survival results for pediatric sufferers. Regular visits to a pediatric eye doctor are essential for early detection and management of vision issues in kids. Post-Resuscitation Care for Pediatric Patients Once a child regains a pulse and respiratory, submit-resuscitation care is vital to:✅ Prevent brain damage – Hypothermia therapy may be used in select instances.✅ Ensure right oxygenation – Monitoring breathing characteristics.✅ Manage underlying situations – Evaluate the reason for arrest (e.g., coronary heart defects, respiratory infections).✅ Monitor for complications – Addressing arrhythmias, organ disorders, and neurological troubles.A pediatric cardiologist can be involved in assessing if the cardiac arrest was because of an underlying coronary heart circumstance. Parents should be aware of pediatric headache red flags to differentiate between common headaches and those requiring immediate attention. Hospital-Based Interventions for Pediatric Cardiac Arrest Survivors Individuals exploring a career in pediatric nursing often research pediatric nurse salary to understand potential earnings in this rewarding field. Once at the sanatorium, youngsters who live to tell the tale of cardiac arrest undergo specialized pediatric care, inclusive of:🏥 Advanced Cardiac Life Support (ACLS): Continuous cardiac and respiratory monitoring.🏥 Neurological Evaluations: Checking for brain features and healing.🏥 Respiratory Support: Ventilation or oxygen therapy if needed.🏥 Cardiac Testing: EKG, echocardiogram, and consultation with a pediatric heart specialist.🏥 Rehabilitation Services: Physical and occupational remedy for motor and cognitive recuperation.A pediatric dermatologist can also evaluate skin situations due to prolonged hypoxia or metabolic modifications. Families rely on PM Pediatric Urgent Care for convenient and expert care during evenings and weekends. Common Challenges in Pediatric Out-of-Hospital Resuscitation Pediatric cardiac arrest offers particular demanding situations compared to personal resuscitation, inclusive of:❌ Delayed reputation of misery – Many bystanders fail to understand early symptoms of respiratory distress.❌ Lack of AED availability – Pediatric-suitable AEDs are not widely on hand.❌ Inadequate CPR knowledge – Many caregivers hesitate to do CPR on children.❌ Emotional pressure – Resuscitating a baby is emotionally overwhelming for both bystanders and experts.Better schooling and attention can assist in triumph over these challenges and enhance pediatric emergency response. Engaging in pediatric physical therapy helps children achieve greater independence and improved quality of life. The Role of Bystanders in Pediatric Emergencies 💡 Bystanders play a vital position in saving kids’s lives. When pediatric cardiac arrest happens, bystanders have to:✔️ Recognize misery early – Observe breathing, responsiveness, and color modifications.✔️ Activate EMS at once – Call 911 without hesitation.✔️ Start CPR and rescue respiration – Provide excellent chest compressions and airflow.✔️ Use an AED if available – If no pulse is detected and the child is unresponsive.Even without formal education, appearing CPR without delay can double survival prices. Those interested in becoming a pediatric CNA should pursue specialized training to work effectively with children in healthcare settings. Community Training and Awareness for Pediatric Emergency Response To enhance pediatric survival rates, groups need to pay attention to the following:📌 Basic CPR schooling – Encouraging faculties, daycare centers, and parents to study pediatric CPR.📌 AED accessibility – Ensuring public places have pediatric-well-suited AEDs.📌 Recognizing pediatric emergencies – Educating caregivers about early warning signs.📌 Integrating pediatric emergency education into healthcare roles – Including pediatric CNAs, nurses, and EMTs.Many centers, together with pediatric ENT clinics, pressing care centers, and pediatric dentistry places of work, need to additionally teach their personnel to respond to medical emergencies involving kids. Improving Survival Rates Through Education and Preparedness 📊 Ways to Improve Pediatric Survival Rates:✔️ Expand CPR and AED education programs for mothers, fathers, and caregivers.✔️ Increase recognition of pediatric assessment equipment just like the Pediatric Assessment Triangle.✔️ Ensure quicker EMS reaction instances and medical institution interventions.✔️ Encourage pediatric healthcare carriers to train in emergency reactions.✔️ Provide AEDs in faculties, playgrounds, and childcare centers.By increasing education, training, and preparedness, we are able to save a greater number of children’s lives throughout cardiac and respiration emergencies. Consulting a pediatric gastroenterologist is essential for managing complex gastrointestinal conditions in pediatric patients. Conclusion: Strengthening the Pediatric Chain of Survival The Pediatric Chain of Survival is the simplest and most robust because of the understanding and actions of the network. From bystanders to EMS vendors and health center teams, each step is subject to improving survival costs.💡 Key Takeaways:✔️ Early recognition of breathing misery prevents cardiac arrest.✔️ Immediate CPR and rescue respiratory are important in pediatric resuscitation.✔️ Defibrillation needs to be performed ASAP for shockable rhythms.✔️ EMS and health facility groups provide specialized pediatric put-up-resuscitation care.✔️ Community training in pediatric CPR and AED use can save more lives.By improving awareness, preparedness, and rapid intervention, we can create a stronger and more powerful pediatric emergency reaction system. Through pediatric occupational therapy, children with physical, sensory, or cognitive challenges can enhance their functional abilities. Disclaimer:Content on Sanford Pharmacy is meant for general information and should not be seen as medical advice. Please consult a licensed healthcare provider before using any medicine. Self-treatment without guidance is not recommended.
Emergency and General Healthcare
Common Medication Mistakes & How to Avoid Them?
 Brendan
Brendan
Disclaimer:Content on Sanford Pharmacy is meant for general information and should not be seen as medical advice. Please consult a licensed healthcare provider before using any medicine. Self-treatment without guidance is not recommended. Drug errors are a significant problem in the health care system, which affects the general integrity of the victims, health care, and medical machines. From smaller abroad to extreme headaches, these errors can have serious consequences, long-term life, negative drug reactions, or even deadly. Understanding remedy errors sorts, getting to know the way to save medicinal drug mistakes, and spotting the legal outcomes of medicine errors for nurses are essential in decreasing these dangers.At Sanford Pharmacy, affected person protection is our precedence. Whether you're a healthcare professional, a caregiver, or a patient coping with prescriptions at domestic, understanding prescription mistakes in the pharmacy and mastering what to do if a wrong remedy is given to a patient can prevent severe medical mishaps. What Are Medication Errors? A remedy error takes place whilst there's a lapse within the prescribing, allotting, or management of medication that ends in damage or the potential for harm. These mistakes can stem from miscommunication, human errors, device failures, or negligence.In scientific terminology, incorrectly taking a medication via mistake is referred to as a drug management error. Such errors may be categorized into diverse categories, regularly determined with the aid of the stage at which the error takes place. Common Medication Error Types Understanding the diverse medication error kinds allows us to figure out and mitigate dangers associated with drug management. Some of the maximum commonplace classes consist of: Prescribing Errors – Incorrect drug choice, dosage, or instructions from the healthcare issuer. Dispensing Errors – Mistakes made by pharmacists, consisting of providing the wrong medicinal drug or wrong dosage instructions. Administration Errors – Errors happening whilst an affected person receives the wrong drug, wrong dosage, or wrong path of administration. These 3 classes form the 3 forms of prescription errors, highlighting the crucial ranges where errors can occur. A deeper knowledge of medical error examples guarantees that healthcare specialists and sufferers remain vigilant. Medication Error Examples To understand the actual-world impact, here are a few examples of drug errors that have brought about excessive complications: Incorrect dose error - a nurse administered 10 mg morphine instead of 1 mg due to an incorrect recipe. The definition of incorrect dose errors includes any example where the administered dose varies from the prescribed dose. Look-Alik, Sound-Alik (Lasa) Medication errors - A patient happens to receive the prescribed celebrities (a painkiller reliever). Incorrect passage of administration - a remedy for intravenous use is given orally, the most important to reduce effects or negative reactions. Allergic Reactions Due to Documentation Errors – An affected person with a documented penicillin hypersensitive reaction is prescribed amoxicillin, resulting in anaphylactic surprise. Each of these medicine mistakes examples underscores the importance of meticulous verification at each level of drug management. How to Prevent Medication Errors Preventing medicinal drug mishaps requires a multifaceted method that consists of stringent safety protocols, continuous training, and technological interventions. Best Practices for Prevention Patient Education – Patients have to be well-knowledgeable approximately their medications, which include their purpose, dosage, and ability facet consequences. Electronic Prescriptions – Using digital health records (EHRs) minimizes misinterpretations resulting from illegible handwriting. Double-Check Protocols – Nurses and pharmacists ought to confirm prescriptions with at least two resources earlier than management. Barcode Scanning Systems – Ensuring that the right medicinal drug reaches the right affected person through the use of barcode verification. Reducing Workload Fatigue – Studies have proven that prescription errors in pharmacy frequently occur because of pharmacist fatigue. Implementing working-hour rules can substantially lessen errors. By following those recommendations, healthcare vendors can substantially lower the risk of medicine error kinds. What to Do If Wrong Medication Given to Patient Despite precautions, mistakes can still arise. Knowing what to do if the wrong medicine is given to a patient can suggest the distinction between swift healing and life-threatening complications. Immediate Actions to Take Assess the Patient – Check for fast unfavorable reactions or signs of misery. Inform the Healthcare Team – Reporting the error ensures that scientific intervention is furnished if needed. Document the Error – Recording information about the mistake can assist in fine development measures. Communicate with the Patient or Family – Transparency is vital in preserving belief and making sure of proper compliance with care. Prompt corrective motion mitigates the ability to harm and improves patient results. Legal Consequences of Medication Errors for Nurses Nurses play an important position in medicine management, making them specifically susceptible to criminal ramifications when errors occur. The prison results of medication errors for nurses vary depending on the severity of the mistake and whether negligence became involved. Potential Legal Repercussions Disciplinary Action – Nurses may also face suspension, retraining requirements, or even job termination. Malpractice Lawsuits – Severe mistakes main to cause personal harm can result in lawsuits, which can be high-priced and unfavorable to a nurse’s expert reputation. Criminal Charges – In cases of gross negligence, criminal charges may be filed, probably leading to fines or imprisonment. License Revocation – Repeated medicinal drug mistakes may additionally lead to a permanent lack of nursing licensure. Understanding the effects of medication errors on nurses underscores the need for rigorous adherence to protection protocols. List Four Actions You Should Take If You Make an Error When Administering Medication If a healthcare expert makes a medicine blunder, positive moves ought to be taken immediately to reduce damage. The following is a list of the moves you ought to take if you make a mistake whilst administering medicine: Report the Incident Immediately – Transparency is vital to address the problem directly. Monitor the Patient Closely – Identify any signs of distress or destructive reactions. Follow Institutional Guidelines – Every healthcare facility has protocols in location for managing medicinal drug mistakes. Participate in Root Cause Analysis – Understanding how the error happened enables in preventing future errors. Final Thoughts: Prioritizing Medication Safety Medication errors pose good-sized dangers, however, with stringent precautions and proper training, they may be minimized. Patients and healthcare carriers alike need to continue to be vigilant, adopting first-class practices for safe remedy coping.Sanford Pharmacy is committed to ensuring safe and accurate remedy distribution. You can conveniently order your prescriptions online, reducing the probability of prescription errors in the pharmacy. Visit Sanford Pharmacy these days for reliable and expert pharmaceutical offerings.By fostering a way of life of protection, imposing sturdy verification structures, and teaching sufferers and healthcare vendors, medicinal drug mistakes may be appreciably decreased—saving lives and shielding careers inside the technique.Disclaimer:Content on Sanford Pharmacy is meant for general information and should not be seen as medical advice. Please consult a licensed healthcare provider before using any medicine. Self-treatment without guidance is not recommended.